When a patient arrives at area hospitals by ambulance, paramedics must wait until they can transfer care to hospital staff. While that process typically happens fairly quickly in Muskoka, paramedics sometimes encounter delays with low-acuity patients—patients with less-severe injuries or conditions. When that delay exceeds the provincial standard of 30 minutes it is referred to an off-load delay.
Effective Monday, April 25, Muskoka Paramedic Services is implementing a new program, called Fit2Sit, that will help to reduce those delays and get paramedics back into service faster.
The Fit2Sit program will allow paramedics, in consultation with the triage nurse, to transfer low-acuity patients directly to the emergency department waiting room.
MPS, at the request of MAHC, worked with Parry Sound Emergency Medical Services to “develop a local protocol that will allow for the safe direct transfer of identified patients to ED waiting rooms. The partner agencies used feedback from other paramedic services in larger areas to develop the inclusion criteria and operational protocol,” according to a staff report presented at the District’s Health Services Committee on April 21.
Triage nurses at each hospital site will make the final decision on whether a patient may be transferred to the waiting room, and will assume responsibility for the patient prior to paramedic departure. Patients who have higher acuity will remain under paramedic care until transfer of care to hospital staff is completed.
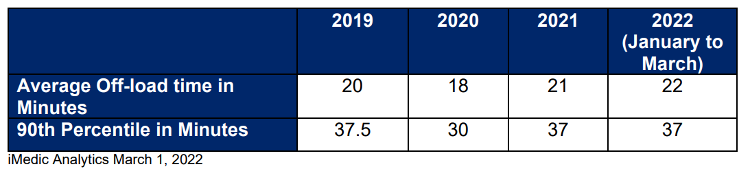
Transfer-of-care times in Muskoka are on average below the 30-minute provincial standard, although there are still a significant number that exceed that mark.
More patients are off-loaded at South Muskoka Memorial Hospital in Bracebridge, which has a slightly higher off-load time, according to the staff report.
In general, off-load times have increased over the last three years, with the exception of 2020 likely due to the
significant reduction in call volume during the early waves of the COVID-19 pandemic.
The following table lists the average off-load time for Muskoka Algonquin Health Centre (MAHC) hospital sites. The 90th percentile row indicates the number of minutes below which 90 per cent of off-load times fall.
“Here in Muskoka, we’ve been pretty lucky and we don’t really experience a lot of off-load delays, and certainly not very often,” said Jeff McWilliam, chief of paramedic services and emergency planning for the District. “The goal is to just turn the paramedics around a little bit quicker with the low-acuity patients that we transport, and therefore have them back in the community to be able to respond to those emergencies.”
McWilliam noted that areas like Niagara, Hamilton, and London, which have higher off-load delays, have implemented a Fit2Sit program and have successfully reduced their paramedic delay times.
In response to a question by Councillor Terry Glover, who is also Lake of Bays mayor, regarding expected call volumes for the summer of 2022, McWilliam said that “historically, we are 25 per cent higher in a regular year of call volume. Noticing the activity as of late—and we can all feel the increase in folks in and around our areas—I anticipate it to probably be a little bit higher. We are already trending higher in 2022…I do anticipate it will be up by 25 per cent if not greater certainly over the seasonal period.”
In a report earlier in the meeting, McWilliam said that MPS received 11,768 calls for service in 2021, and as a result assessed 9,646 people and transported 7,182 patients to an emergency department. In some cases, a patient may have cancelled the request for assistance before paramedics arrived, found alternative transportation, or refused assessment, or may have been deceased.
The five most common emergent and urgent call types in 2021 remained the same as in 2020: trauma/motor vehicle collisions/falls; difficulty breathing; weakness/dizziness/unwell; chest pain; and abdominal pain. Calls for difficulty breathing and feeling unwell did not increase in overall frequency as a result of the pandemic.
Emergency call volume was 18 per cent higher in 2021 compared to 2020, and 14 per cent higher than 2019. MPS typically sees low single-digit call volume increases year over year, according to the staff report, so 2021 represents a significant increase.
Don’t miss out on Doppler!Sign up here to receive our email digest with links to our most recent stories.
Local news in your inbox three times per week!
Click here to support local news


0 Comments